In a new study, researchers explored Alzheimer’s disease and its potential relationship with the estrogen receptor-α gene (ESR1).
The Trending With Impact series highlights Aging publications (listed as “Aging (Albany NY)” by Medline/PubMed and “Aging-US” by Web of Science) that attract higher visibility among readers around the world online, in the news, and on social media—beyond normal readership levels. Look for future science news about the latest trending publications here, and at Aging-US.com.
—
The United States government currently has a mind-blowing annual budget of $3.5 billion designated for Alzheimer’s disease (AD) and dementia research funding. Therapeutics pushed forward thus far have been largely based on the amyloid-beta (Aβ) cascade hypothesis of AD. Surprisingly, despite decades and billions, these interventions have yielded little to no benefits for AD patients. This lack of efficacy has encouraged some researchers to rethink AD pathology and focus on discovering key triggers and mechanisms of neuroinflammation.
“There has been a lengthy and ongoing scientific debate around the causative factors of AD, and the relative importance of both senile Aβ plaques and tau tangles has been largely informed by postmortem investigations of the AD brain. For several decades, the amyloid hypothesis has dominated the field, which has brought forth many high-profile therapeutic attempts that have produced side effects but no real benefits [5].”
Women & Alzheimer’s Disease
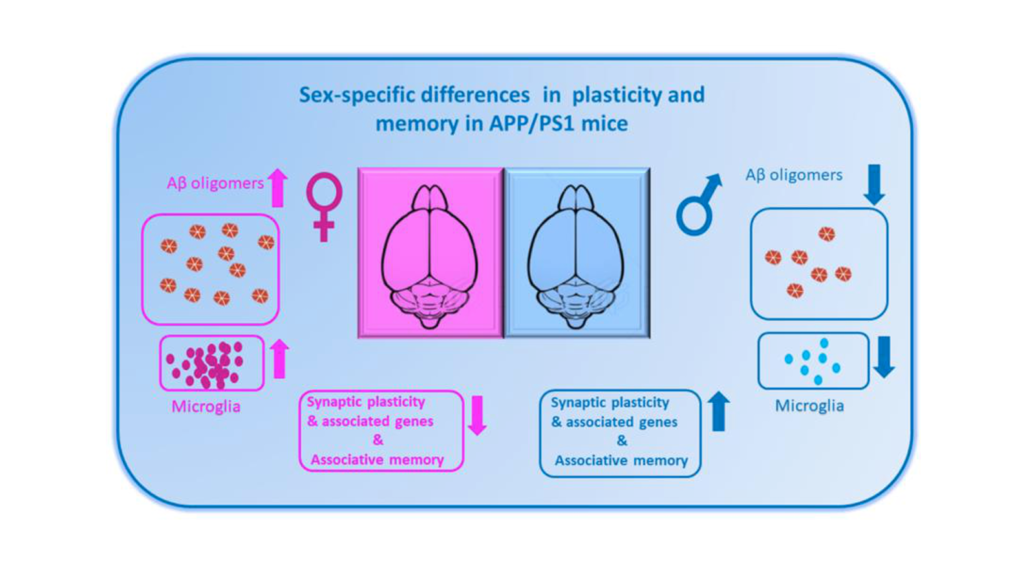
Women compose two-thirds of the United States Alzheimer’s population. Is this gender-specific risk a result of living longer or is it due to other causes, perhaps related to hormonal differences or gender-associated differential gene expression? Previous studies have found that estrogen may protect neurons from the damaging effects of amyloid-beta plaques and tau tangles. However, in women, estrogen levels tend to decline with age, which could be one reason why aging women are more susceptible to AD.
In a new study, researchers Junying Liu, Shouli Yuan, Xinhui Niu, Robbie Kelleher, and Helen Sheridan from Trinity College Dublin, Peking University and Jilin University examined the potential relationship between the estrogen receptor-α gene (ESR1) and neuroinflammation. Their research paper was published on November 1, 2022, in Aging’s Volume 14, Issue 21, and entitled, “ESR1 dysfunction triggers neuroinflammation as a critical upstream causative factor of the Alzheimer’s disease process.”
“AD is characterized by three major questions: Why is age the primary risk factor? Why are women more sensitive to the onset of this form of dementia? And why are neurons in areas of the brain that are essential for memory selectively targeted?”
The Study
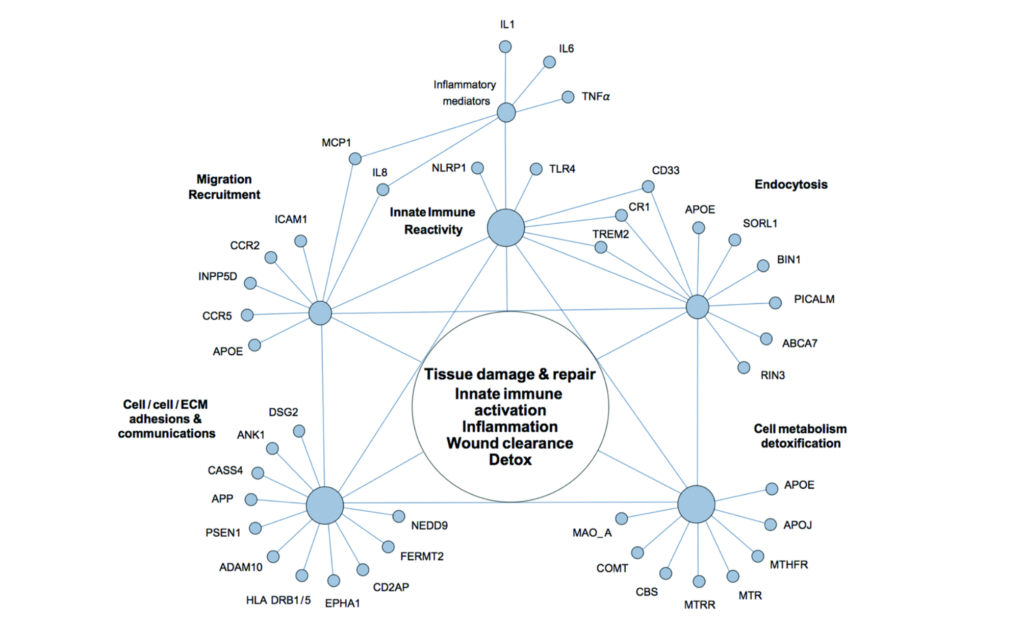
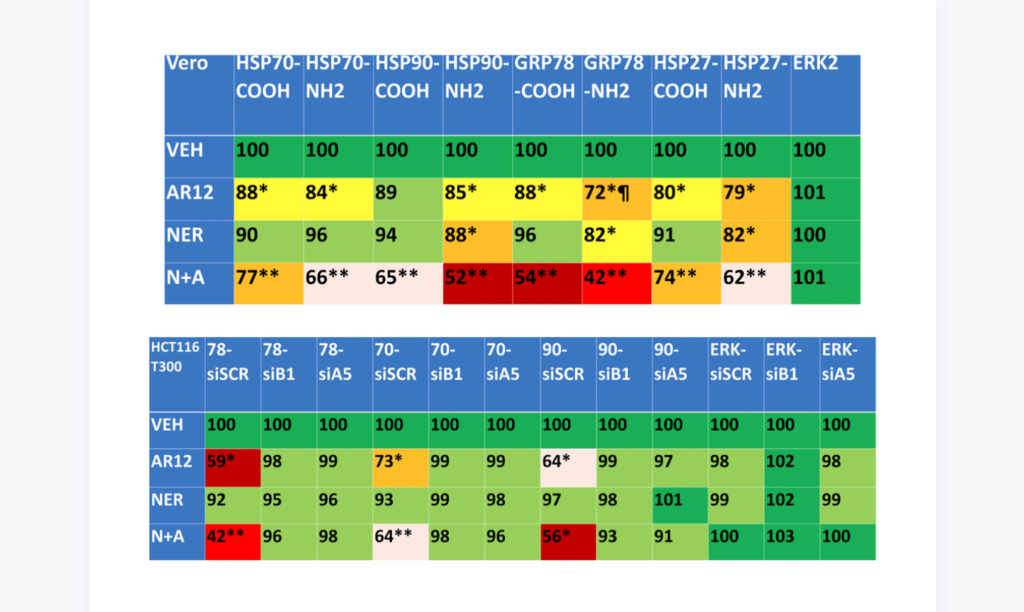
Originally, the researchers in this study had been in the process of investigating ESR1-knockdown in breast cancer when they stumbled upon another discovery. (ESR1 is a gene that codes for the estrogen receptor, a protein that helps to regulate cell division and differentiation.) To their surprise, KEGG pathway enrichment analysis showed that ESR1 may also be related to axonal guidance, inflammation-related gene markers and Notch signaling pathways. Upon further validation using a dataset of in vivo AD inflammatory samples, the team found that the ESR1 gene was altered in AD patients and was associated with an increase in pro-inflammatory markers.
“ESR dysfunction likely plays a role in AD pathology – especially in women – although the specific mechanisms remain unclear. In vivo and ex vivo studies demonstrate that neuroinflammatory brain states overlap with ESR signaling pathways and that these two systems interact closely.”
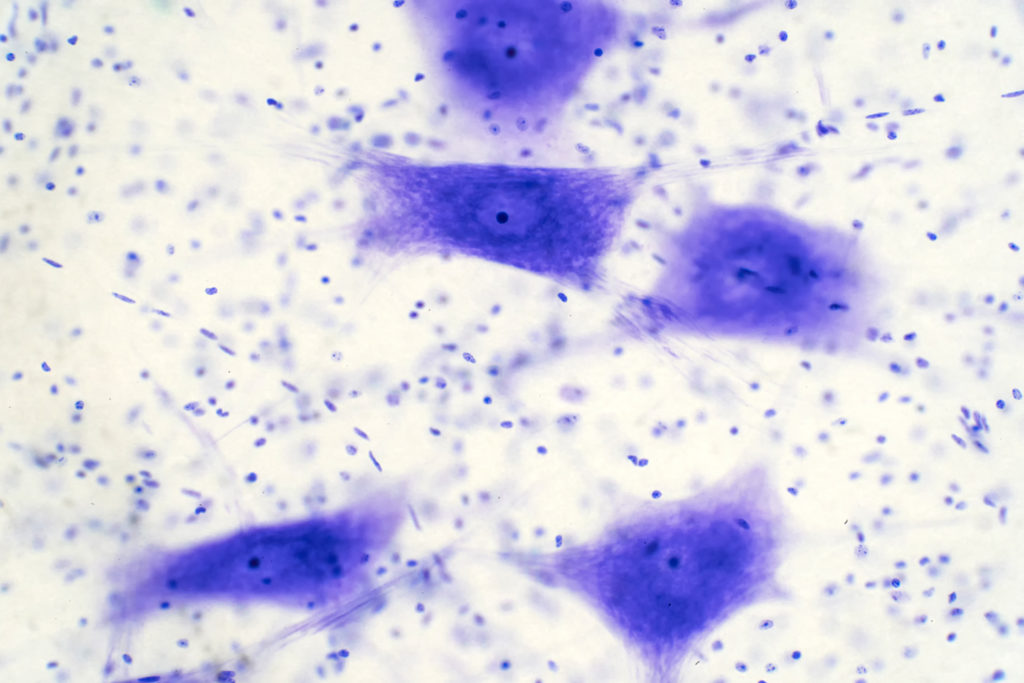
In the current study, the researchers used an animal model to explore the potential role of ESR1 in modulating inflammation-related AD pathology. Using a macrophage cell line, they identified ESR1 as a key modulator of inflammation in the context of AD. They then showed that when the ESR1 gene was absent or mutated, neuroinflammation occurred. This finding offers a potential mechanism for understanding the gender-specific risk of AD in women.
“Our results suggest that ESR1 is modulated by apolipoprotein E (APOE) through CEBPB/ATF4, mir-155-5p, or mir-1-3p. Moreover, sea hare-hydrolysates (SHH), as one of the axonal guidance molecules, could regulate the STAT3/PRDM1/CEBPB pathway and consequently induce cell death through pyroptosis signaling pathways, trigger the secretion of IL1β, leading to neuroinflammation and worsening AD pathogenesis. Molecular docking verification demonstrated that the predicted natural products scoulerine and genistein displayed strong binding affinities for BACE1 and ESR1, respectively. This strategy can be used to design novel, personalized therapeutic approaches to treatment and a first-in-class clinical lead for the personalized treatment of AD.”
Conclusion
The research team concluded that further studies are needed to elucidate the exact mechanisms through which ESR1 modulates inflammation and its role in Alzheimer’s disease. These findings may offer a novel therapeutic direction for treating AD. Therapeutics targeting ESR1 could potentially be used to reduce inflammation in the brain and prevent AD progression. This may be beneficial for both men and women afflicted with this devastating disease.
“Unfortunately, despite enormous efforts, there remains no cure for this terrible illness, and current treatments merely alleviate its devastating symptoms for a short time. This study performed several bioinformatics-based analyses, concluding that ESR1 dysfunction might mediate axonal guidance, induce neuroinflammation or pyroptosis in the brain, and subsequently worsen AD conditions.”
Click here to read the full research paper published by Aging.
AGING (AGING-US) VIDEOS: YouTube | LabTube | Aging-US.com
—
Aging is an open-access journal that publishes research papers bi-monthly in all fields of aging research. These papers are available at no cost to readers on Aging-us.com. Open-access journals have the power to benefit humanity from the inside out by rapidly disseminating information that may be freely shared with researchers, colleagues, family, and friends around the world.
For media inquiries, please contact media@impactjournals.com.