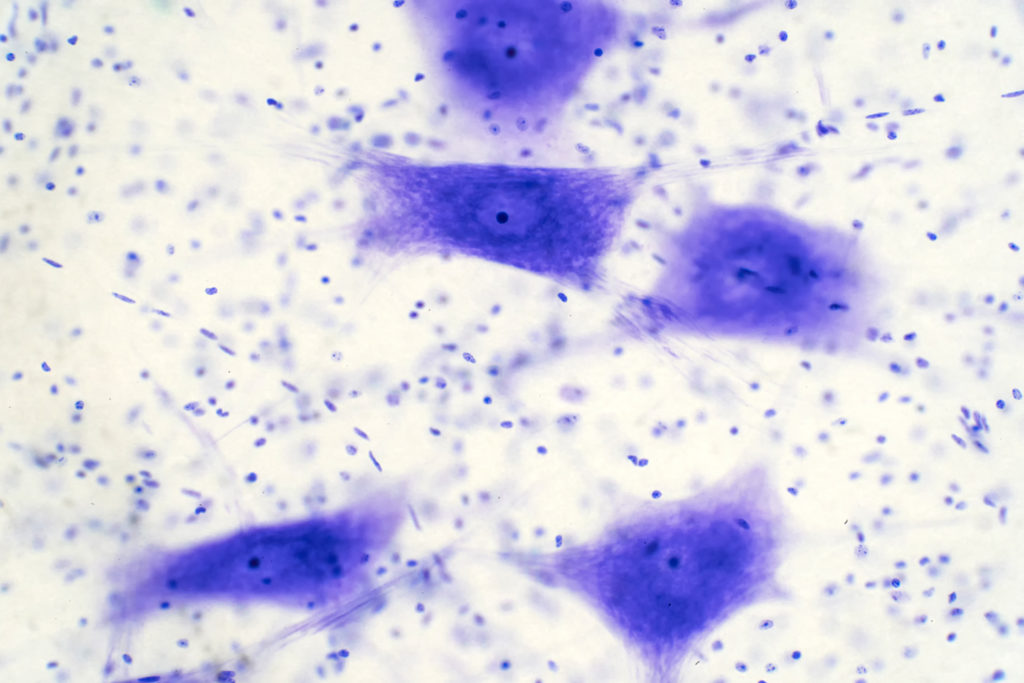
“Cellular senescence is a hallmark of aging and the age-related condition, Alzheimer’s disease (AD).”
Could a class of drugs that clear aging cells also help treat Alzheimer’s disease? A recent study, featured as the cover for Aging (Volume 17, Issue 3), titled “Differential senolytic inhibition of normal versus Aβ-associated cholinesterases: implications in aging and Alzheimer’s disease,” suggests they might—and with remarkable precision.
Understanding Alzheimer’s Disease
Alzheimer’s disease is a progressive neurological disorder that gradually steals memory, independence, and a person’s sense of identity. A defining feature of Alzheimer’s is the buildup of amyloid-β (Aβ) plaques—sticky protein clumps that interfere with communication between brain cells. This disruption is closely linked to changes in a group of enzymes called cholinesterases, especially acetylcholinesterase (AChE) and butyrylcholinesterase (BChE). These enzymes normally play a vital role in regulating neurotransmitters critical for memory, learning, and cognitive function. In Alzheimer’s, however, their behavior changes significantly, particularly when they interact with Aβ plaques.
The Study: Exploring Senolytics for Alzheimer’s Enzyme Inhibition
A research team from Dalhousie University in Canada looked into whether senolytic compounds—a class of drugs that eliminate damaged, aging cells often referred to as “zombie” cells—could also target the harmful forms of cholinesterase enzymes found in Alzheimer’s disease. Their goal was to see if these compounds could selectively inhibit the disease-associated versions of AChE and BChE, without affecting the healthy forms that are essential for normal brain function.
Led by Dr. Sultan Darvesh, the study tested six compounds: five senolytics—dasatinib, nintedanib, fisetin, quercetin, and GW2580—and one nootropic, meclofenoxate hydrochloride, known for its memory-enhancing potential. The researchers used post-mortem brain tissue from Alzheimer’s patients, enzyme activity assays, and computer modeling to examine how these compounds interact with the enzymes.
The Challenge: Targeting the Right Enzymes
One of the limitations of current Alzheimer’s treatments is that they do not distinguish between the normal and the altered forms of cholinesterases. While these drugs can raise levels of the memory-related chemical acetylcholine and improve cognitive function, they often come with side effects due to their broad activity. A more precise approach—targeting only the versions of AChE and BChE tied to Aβ plaques—could offer better outcomes with fewer drawbacks.
The Results: Senolytics Show Precision in Enzyme Targeting
The results were promising. Some of the senolytics tested, like dasatinib and nintedanib, effectively blocked the cholinesterases attached to Aβ plaques without affecting the normal versions of these enzymes in healthy brain tissue. Meclofenoxate also showed strong activity against the disease-associated forms. Interestingly, this selectivity was linked to how these compounds bind to the enzymes. Instead of locking onto the main active site, many of them attached to alternative regions, known as allosteric sites, which are only altered in the plaque-associated forms. This type of binding allowed the compounds to distinguish between harmful and healthy enzymes.
The Breakthrough: Targeting the Disease, Preserving the Brain
This study is the first to show that certain senolytic and cognitive-enhancing drugs can selectively inhibit the dysfunctional versions of cholinesterases found in Alzheimer’s without affecting their normal forms. This level of precision could mark a major step forward in Alzheimer’s therapy.
The Impact: A Dual-Action Path to Treating Alzheimer’s
By focusing on only the problematic forms of AChE and BChE, this approach could lead to Alzheimer’s treatments that better preserve cognitive function while avoiding side effects. The research also bridges two important areas of study: aging and neurodegeneration. It suggests that drugs developed to slow aging might also be used as targeted treatments for Alzheimer’s, offering a two-in-one therapeutic advantage.
Future Perspectives and Conclusion
Although more research is needed, especially in living models and clinical trials, the potential of the findings is encouraging. They lead the way for a new generation of Alzheimer’s treatments that are more targeted and safer.
By understanding better how aging and brain disease intersect at the cellular level, scientists may be moving closer to developing more effective and personalized approaches to combat Alzheimer’s.
Click here to read the full research paper in Aging.
___
Aging is indexed by PubMed/Medline (abbreviated as “Aging (Albany NY)”), PubMed Central, Web of Science: Science Citation Index Expanded (abbreviated as “Aging‐US” and listed in the Cell Biology and Geriatrics & Gerontology categories), Scopus (abbreviated as “Aging” and listed in the Cell Biology and Aging categories), Biological Abstracts, BIOSIS Previews, EMBASE, META (Chan Zuckerberg Initiative) (2018-2022), and Dimensions (Digital Science).
Click here to subscribe to Aging publication updates.
For media inquiries, please contact [email protected].
![Figure 1. The EORS downward spiral of aging and Alzheimer’s (Epigenetic Oxidative Redox Shift) [2].](/wp-content/uploads/2021/06/Screen-Shot-2021-06-24-at-4.27.37-PM-1024x636.png)