In 2020, researchers conducted an analysis of multimodal data on Alzheimer’s disease (AD). Their research concluded that AD may not begin with amyloid-β.
The Trending with Impact series highlights Aging (Aging-US) publications that attract higher visibility among readers around the world online, in the news, and on social media—beyond normal readership levels. Look for future science news about the latest trending publications here, and at Aging-US.com.
—
The root cause of Alzheimer’s disease (AD) is still unknown. For the past decades, the dominant paradigm many scientists have based their AD therapeutic solutions on has been the amyloid cascade hypothesis. The amyloid cascade hypothesis proposes that AD begins with the overproduction and accumulation of amyloid-β, followed by a number of other cascading symptoms. However, over 200 drug candidates based on this model have failed to prove clinical benefits in trial phases.
“The unsettlingly consistent failure of clinical trials led to questioning of the amyloid cascade hypothesis, stimulating a search for alternative AD paradigms [10–13].”
Researchers Alexei Kurakin and Dale E. Bredesen, from the University of California Los Angeles and the Buck Institute for Research on Aging, conducted detailed analyses of early-stage AD patient data and concluded their study by offering an alternative AD hypothesis. Their paper, published by Aging (Aging-US) in 2020, was entitled, “Alzheimer’s disease as a systems network disorder: chronic stress/dyshomeostasis, innate immunity, and genetics.”
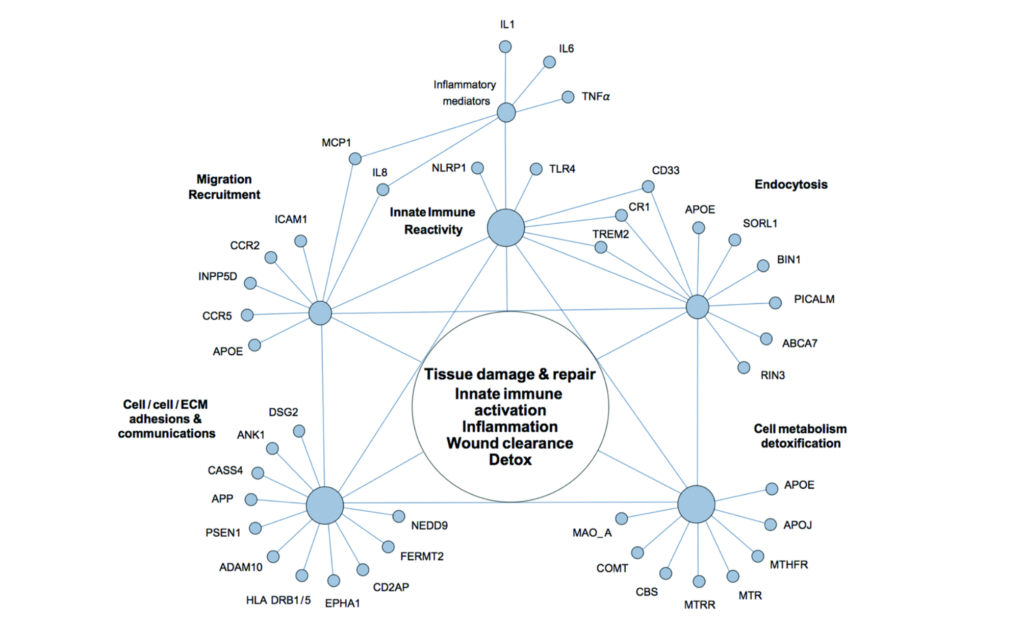
“In this report, we outline an alternative perspective on AD as a systems network disorder and discuss biochemical and genetic evidence suggesting the central role of chronic tissue injury/dyshomeostasis, innate immune reactivity, and inflammation in the etiopathobiology of Alzheimer’s disease.”
THE STUDY
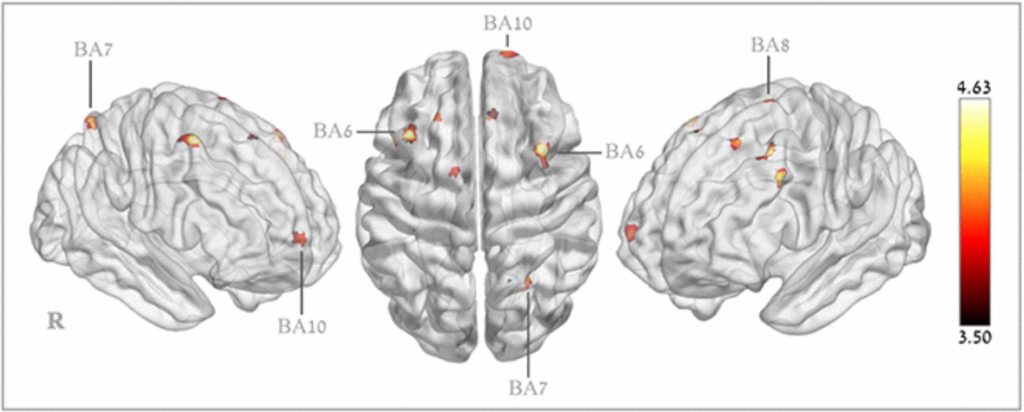
The researchers attempted to conduct an unbiased analysis of clinical profiles of early-stage Alzheimer’s disease patients and accumulated research data. Their search algorithms were hypothesis-independent and they used “expert assistance” to synthesize multimodal data. A list of AD plasma biomarkers were compared with classical acute-phase response reactants. A network of genetic polymorphisms associated with AD were aggregated in addition to a quick reference guide for select AD susceptibility factors. In totality, their expansive research and organization of accumulated data has led them to conclude that Alzheimer’s disease may be a system-level network disorder.
“Reconciling multimodal clinical profiles of early-stage AD patients and research knowledge accumulated in diverse expert domains suggests that sporadic Alzheimer’s disease may not be a homogenous CNS disease, but a heterogeneous, system-level, network disorder, which is driven by chronic network stress and dyshomeostasis.”
CONCLUSION
Key structures and circuits of the central nervous system may be preferential targets of AD symptoms, including chronic systemic stress, toxicity and inflammation. The researchers believe this is mainly due to the central nervous system’s centric positions and functions. In AD, symptoms are initially highly heterogeneous until the disease reaches its “endpoint,” which is recognized as Alzheimer’s disease. This may be the reason that treating AD with monotherapies has not yet yielded effective results.
Given this new model of viewing Alzheimer’s disease as a system-level network disorder, the researchers propose that patients should be treated using precision medicine tactics. Dr. Bredesen has developed a novel therapeutic approach designed to treat each individual patient for their unique symptoms of cognitive decline and Alzheimer’s disease. Using the Bredeson Protocol, many patients have reported years of improved, and even reversed, cognitive decline. Dr. Bredesen also notes in a recent Aging Interview that it is important to treat early signs of AD, just as it is important to detect other diseases in early stages.
“The promising results of an integrative, systemic, precision medicine approach to treating Alzheimer’s disease suggests that evaluating and addressing the individual organism as a whole rather than focusing exclusively on an apparently failing part may represent a promising strategy to approach other complex chronic multifactorial disorders, which warrants further exploration and development.”
Click here to read the full research paper, published by Aging.
WATCH: AGING VIDEOS ON LABTUBE
—
Aging is an open-access journal that publishes research papers monthly in all fields of aging research and other topics. These papers are available to read at no cost to readers on Aging-us.com. Open-access journals offer information that has the potential to benefit our societies from the inside out and may be shared with friends, neighbors, colleagues, and other researchers, far and wide.
For media inquiries, please contact [email protected].