The MEND (Bredesen) protocol to treat neurodegeneration associated with Alzheimer’s disease was tested in a small cohort. In 2016, researchers followed up with objective results.
The Top-Performer series highlights papers published by Aging that have generated a high Altmetric Attention score. Altmetric scores, located at the top-left of trending Aging papers, provide an at-a-glance indication of the volume and type of online attention the research has received.
Read Aging’s Top 100 Altmetric papers.
—
Precursors to the onset of early Alzheimer’s disease (AD) include mild cognitive impairment (MCI) and subjective cognitive impairment (SCI). Many have viewed this looming neurodegeneration as an unavoidable fate that accompanies aging. However, in a 2014 study, a novel precision medicine treatment approach, termed the metabolic enhancement for neurodegeneration (MEND) protocol, yielded unprecedented results. Nine out of 10 participants with memory loss associated with AD, amnestic MCI, and SCI, were treated using the MEND protocol. Participants displayed subjective improvement in cognition within 3-6 months of this protocol. The study claims their only failure was one patient with very late stage AD.
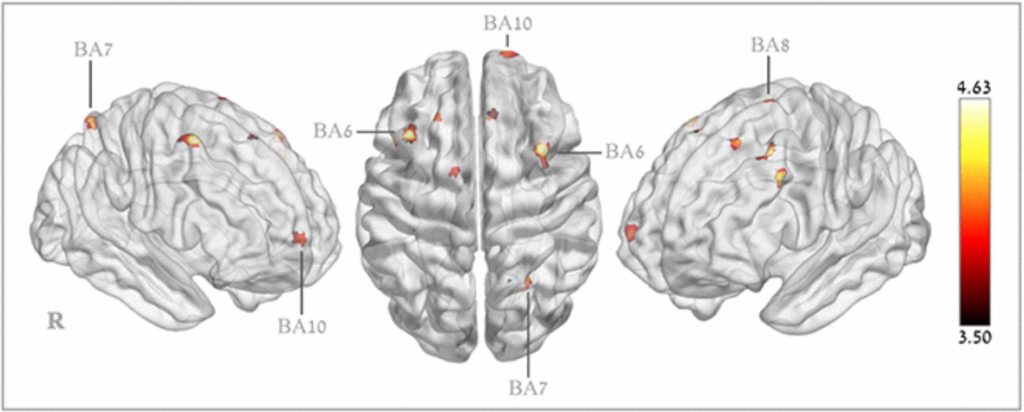
In 2016, researchers—from the University of California, Buck Institute for Research on Aging, Pacific Medical Center, and Brainreader—followed up on the anecdotal results from the 10 patients in this study. They provided objective results from quantitative magnetic resonance imaging (MRI) and neuropsychological testing. The researchers authored another paper on results of the MEND protocol, which was published by Aging and entitled, “Reversal of cognitive decline in Alzheimer’s disease.” To date, this paper has generated an Altmetric Attention score of 263. The original 2014 paper on the MEND study has also generated an impressive Altmetric Attention score of 470.
“In each of these cases, obvious subjective improvement, noted by the patient, his/her significant other, and his/her co-workers, was accompanied by clear, quantitated, objective improvement.”
THE MEND PROTOCOL
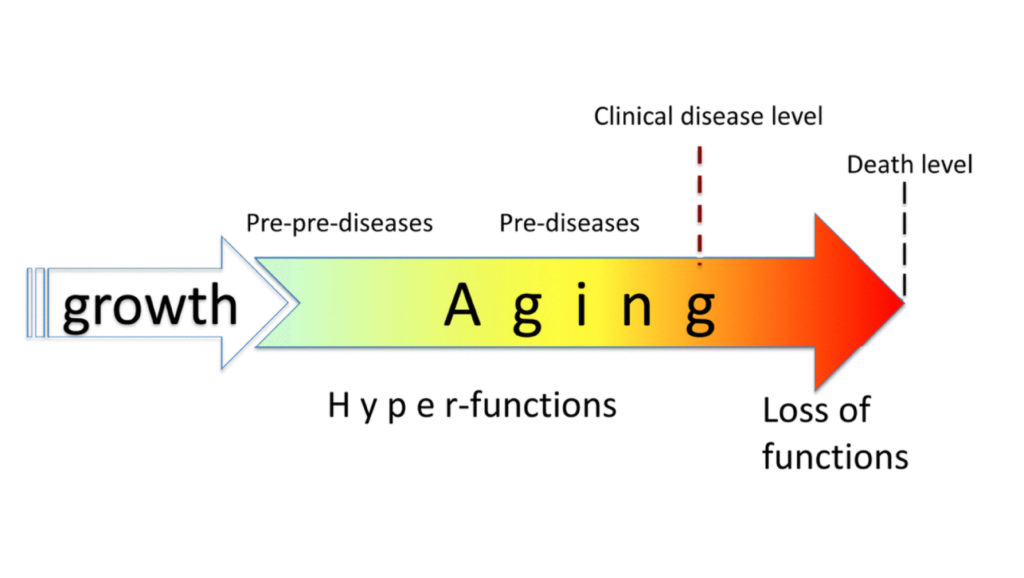
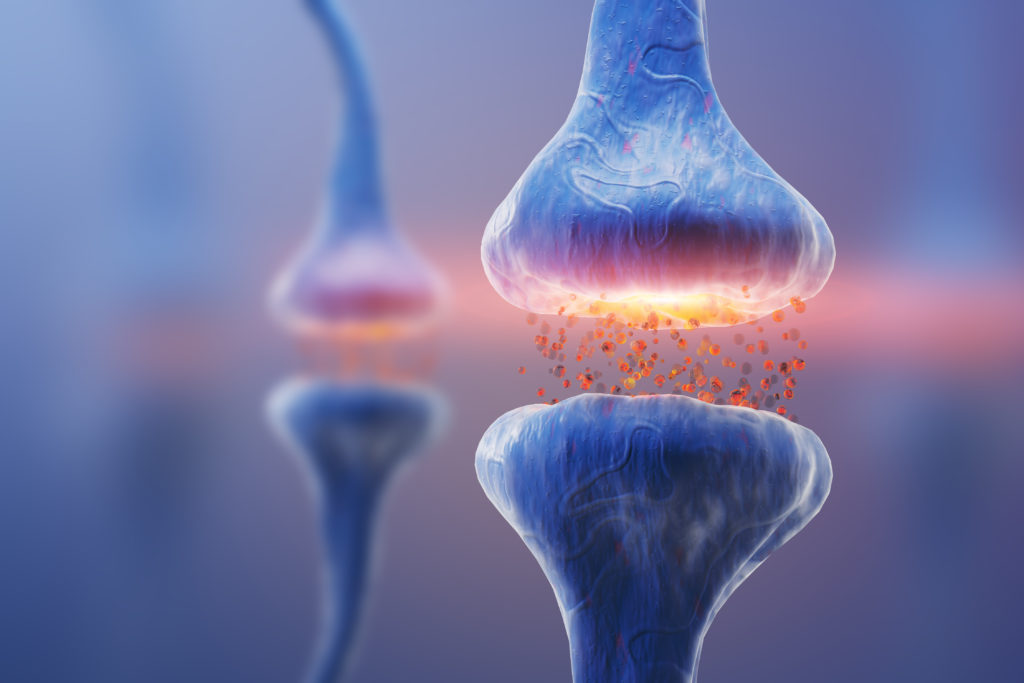
The MEND protocol, also known as the Bredesen Protocol (named after the creator of the protocol, Dr. Dale Bredesen), consists of a multifaceted, tailored approach to treating each AD patient for their individual symptoms of cognitive decline—and not only a few symptoms. This strategy uses a combination of diet, lifestyle, and therapeutic interventions. Treatment is based on the hypothesis that AD occurs due to an imbalance in an extensive plasticity network in the brain. The authors note that the MEND protocol is an iterative process and designed to improve with continued patient visits.
“The therapeutic system described in this report derives from basic studies of the role of APP signaling and proteolysis in plasticity, and the imbalance in this receptor proteolysis that reproducibly occurs in Alzheimer’s disease.”
Upon clinical assessment and lab testing, the patients’ physical and cognitive health were evaluated. Based on this assessment, patients were prescribed a lengthy personalized therapeutic system. Among other objectives, the MEND protocol recommends treating diabetes; improving sleep and digestive health; reducing stress, inflammation, and blood sugar; increasing physical exercise, intellectual stimulation, antioxidants, and vitamins; and optimizing hormone balance, synthesis of acetylcholine, nerve growth factors and mitochondrial function.
ANECDOTAL AND OBJECTIVE RESULTS
“The magnitude of the improvement is unprecedented, providing additional objective evidence that this programmatic approach to cognitive decline is highly effective.”
Before participating in the MEND protocol, most of the 10 participants reported a family history of AD, confusion, difficulty with word finding, following instructions, remembering, reading, concentrating, driving, completing work related tasks, and other cognitive struggles. Over the course of between five and 24 months on the MEND, nine of 10 patients and their families or caregivers reported improved cognitive function. Some patients were able to go back to work, play games, and even babysit their grandchildren. One spouse of a patient mentioned that her husband had stopped following the protocol for a period of time, which resulted in him leaving the car in the driveway idling with the keys in the ignition. After he resumed the protocol, no such instances were reported.
Bearing in mind that this study used an extremely small cohort to test this very expensive protocol, the objective results observed by the researchers were still considerably significant. Quantitative neuropsychological testing showed improvements of up to three standard deviations. One patient showed an increase in hippocampal volume from 17th percentile to 75th percentile. These results must be verified in a larger sample size to validate efficacy.
CONCLUSION
“The initial results for these patients show greater improvements than have been reported for other patients treated for Alzheimer’s disease. The results provide further support for the suggestion that such a comprehensive approach [3] to treat early Alzheimer’s disease and its precursors, MCI and SCI, is effective. The results also support the need for a large-scale, personalized clinical trial using this protocol.”
Click here to read the full research paper, published by Aging.
WATCH: MORE AGING VIDEOS ON LABTUBE
—
Aging is an open-access journal that publishes research papers monthly in all fields of aging research and other topics. These papers are available to read at no cost to readers on Aging-us.com. Open-access journals offer information that has the potential to benefit our societies from the inside out and may be shared with friends, neighbors, colleagues, and other researchers, far and wide.
For media inquiries, please contact [email protected].