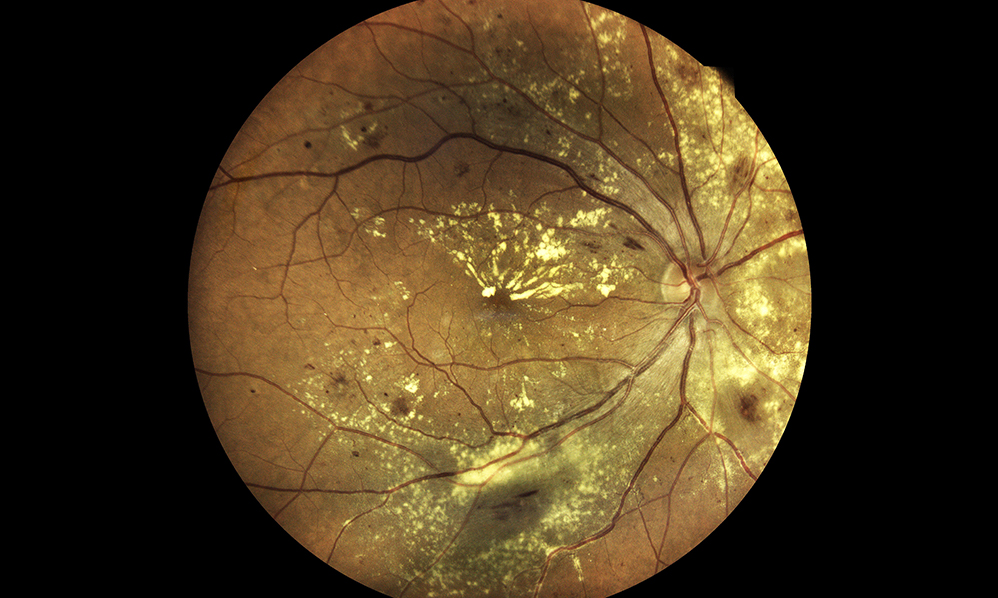
Over 15 million people in the United States are currently struggling with age-related macular degeneration (AMD). Among aging populations around the world, AMD is the leading cause of irreversible vision loss. A main target of AMD is the pigmented layer of the retina, or the retinal pigment epithelium (RPE). The subretinal space of the eye encompasses the area under the retina between RPE cells and photoreceptors. Yellow deposits of lipids and proteins, called drusen, are located in the subretinal space and the hallmark sign of AMD. In 2005, researchers found that drusen deposits also contain an immune protein called the C-reactive protein (CRP).
Circulating CRP is one of the main clinical biomarkers of inflammation and infection, since CRP levels rise and fall with inflammation. This immune-response protein can exert pro-inflammatory properties by disassociating from its pentameric form (pCRP) into smaller monomeric CRP (mCRP) subunits. These mCRPs are small enough to cross the ocular blood–retinal barrier (oBRB) and appear in ocular drusen.
“mCRP has been identified in ocular drusen and other subepithelial deposits [24, 25], as well as in the choroid, and we have shown that mCRP, but not pCRP, contributes to oBRB disruption in vitro [26].”
Researchers—from Hospital Clínic de Barcelona, Manchester Metropolitan University, Hospital de la Santa Creu i Sant Pau, Institute Salud Carlos III, University of Bristol, Moorfields Eye Hospital, and University College London Institute of Ophthalmology—conducted a study aimed at understanding the mCRP’s contribution to the pathophysiology of AMD. Their paper was published by Aging (Aging-US) in 2020, and entitled, “Activation of C-reactive protein proinflammatory phenotype in the blood retinal barrier in vitro: implications for age-related macular degeneration”.
The Study
“If mCRP pro-inflammatory capacity is unrestrained in AMD and particularly in high risk patients, then we need to determine how mCRP is generated or accumulates in the subretinal space as there is no CRP transcription in the retinal tissue [30, 31].”
In order to investigate how mCRP is generated and/or how it accumulates within the subretinal space, the researchers used a Transwell model to first determine whether circulating CRP could reach the subretinal space. The Transwell model included monolayers of primary porcine choroidal endothelial cells (CECs) grown on porous filters with their apical and basolateral surfaces exposed to separate chambers. They found that CRP isoforms were able to cross the CEC monolayer on the apical side of the RPE. Next, they used the Transwell model to evaluate whether CRP isoforms could also reach the subretinal space and cross RPE ARPE-19 cells. They found that mCRP was able to diffuse into both the subretinal space and cross into the RPE. pCRP was not found in the opposite chambers, even after 24 and 48 hours post-exposure. However, when the researchers tested younger and healthier primary porcine RPE cells instead of the ARPE-19 cells, neither pCRP nor mCRP diffused into opposite chambers.
Next, the researchers studied whether pCRP could dissociate into mCRP within the RPE. They found that induced inflammation triggered pCRP dissociation into mCRP in both the ARPE-19 and primary porcine RPE cells. The team also found that barrier disruption induced by mCRP was dependent on its topological localization.
Conclusion
“In summary, our findings further support mCRP direct contribution to progression of AMD, at least at the RPE level. The topological experiments elicit that mCRP is proinflammatory when present on the apical side of the RPE. However, mCRP is likely to only reach the apical side of the RPE in compromised RPE health and where barrier functions are compromised.”
The researchers were forthcoming about limitations in their study. Nonetheless, this study suggests that a plausible mechanism by which mCRP may contribute to RPE dysfunction and AMD progression is, when pCRP reaches the oBRB, it diffuses past the oBRB by dissociating into mCRP. It is also possible that mCRP may be derived from the dissociation of pCRP on the surface of damaged RPE. The proinflammatory microenvironment may be amplified and the barrier disruption may be enhanced when mCRP reaches the apical side of an already aged or damaged RPE.
“With respect to previous findings, this pathologic mechanism will be more prevalent in patients carrying the FH risk polymorphism for AMD, where mCRP proinflammatory effects remain unrestrained [28].”
Click here to read the full research paper published by Aging (Aging-US).
AGING (AGING-US) VIDEOS: YouTube | LabTube | Aging-US.com
—
Aging (Aging-US) is an open-access journal that publishes research papers bi-monthly in all fields of aging research and other topics. These papers are available to read at no cost to readers on Aging-us.com. Open-access journals offer information that has the potential to benefit our societies from the inside out and may be shared with friends, neighbors, colleagues, and other researchers, far and wide.
For media inquiries, please contact [email protected].