Dr. David Sinclair from Harvard Medical School and member of the Aging Editorial Board details his review published by Aging on May 29, 2020, entitled, “Why does COVID-19 disproportionately affect older people?“

Behind the Study is a series of transcribed videos from researchers elaborating on their recent oncology-focused studies published by Aging. Visit the Aging YouTube channel for more insights from outstanding authors.
—
It’s David Sinclair here. I’m talking to you from my home in Boston during this pandemic stayed home time, but also wanted to talk to you about a new paper that we have coming out, or just came out in our journal, Aging, and its title is, “Why Does COVID-19 Disproportionately Affect the Elderly?”—which has become one of the biggest questions I think in this whole pandemic. And, if we could understand why the elderly were more susceptible, first of all, we could help them survive and have less severe cases, but also we could learn perhaps why younger people are also more susceptible. One thing that I often hear when I pose that question is oh, it’s just that old people are sicker and they die. Well, that’s not a good enough explanation because the elderly, even if they are healthy, have a much greater chance of dying than someone whose say, less than 65.
In fact, of all the main causes of death or risk factors in COVID-19, age is by far the most important one, independent of all those other risk factors. So a study just came out in the UK that looked at 17 million people that had COVID-19 and they could tell us based on that, what the ranking of the what’s called the hazard ratio of which symptoms and which lifestyle and cobalt morbidities track with COVID-19 more fatality risk.
And actually, in order starting with number five, it was diabetes/obesity. Number three was being male, that’s fairly risky. Having cancer of the blood was bad, which makes sense because you’ve disrupted your immune system. But by far the riskiest thing is age, independent of all these other things. In fact, compared to these other risks, age is basically the major determinate. If you’re 80, numbers where you’re about tenfold higher to someone who’s in their late 50s. So that led us to try to figure out what is going on with the age that makes them more susceptible. And again, it’s not just that those people start out sicker. And so we’ve written this perspective and gathered a lot of data from around the world, papers that have come out, papers that have been in publication. So in this perspective, we’ve gathered a lot of data from around the world, new papers, old papers, and really put together a list of things that we think are the most likely explanations for the elderly succumbing to COVID-19, independent of their actual underlying diseases and frailty.
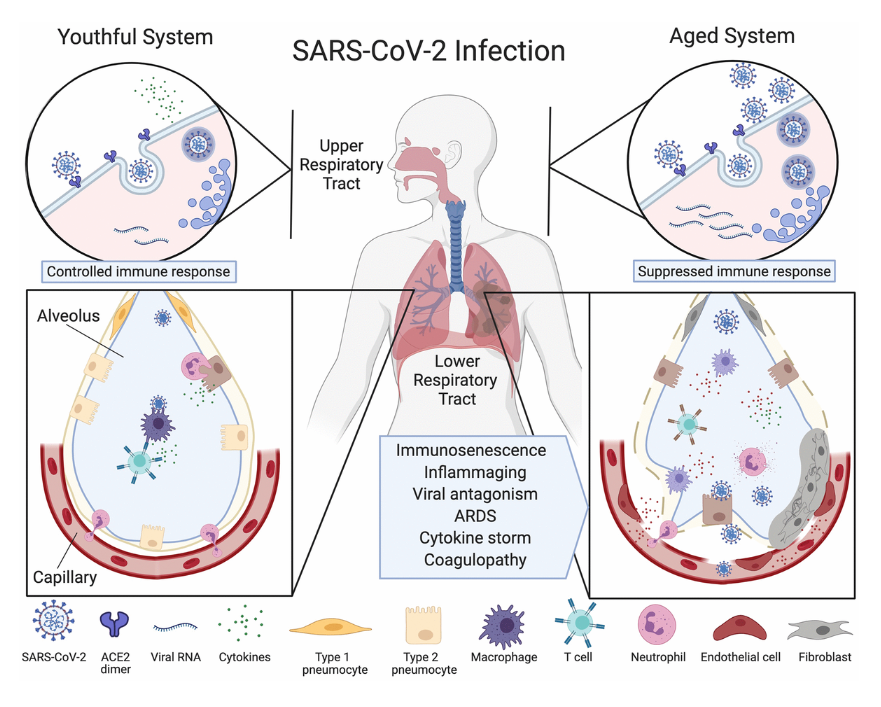
So let’s first go through one of the figures—you’ll see figure one is a beautiful illustration drawn by my wonderful coauthors, Amber Mueller and Maeve McNamara. And it’s a picture of what goes wrong in the elderly compared to someone who can clear the infection. And what you’ll see is that there’s a cut through the lung. And what happens in the elderly is that the virus goes down into the lung, causes hyper immune response. And in the late stages of the disease in the elderly particularly, it’s a hyper immune response, which we call the cytokine storm. And what we’ve recently discovered, the planet that is not just my lab, is that the virus can attack the endothelial cells of the agent. And that’s not just in the lung, which of course is a problem for getting blood flow and oxygen across, but what’s also important is that these endothelial cells that line the blood vessels, particularly the micro capillaries, line at the heart, the brain, even the extremities.
And so what we’re seeing in elderly patients particularly that undergo this cytokine storm is what’s called a coagulopathy, which means that lining of the blood vessels is getting inflamed and causing clots to form. And you get a rise in this marker called the D-dimer, which is a breakdown product of clotting. And what we’re seeing is even in young people, there’s propensity for stroke, myocardial infarction, heart attack, and even things like numbing of the toes and the fingers. And you can see that there are what are called chilblains in some people, you get these dark areas on the body. So that’s particularly fatal if it’s not controlled and it’s very difficult to control that. So what’s behind all of this susceptibility to the agent?
Well, there are two things going on, mainly one is the inability to clear the virus initially. So if you’re young, you can have a spike in viral numbers. It starts to get in your throat, drift down into the lungs. But young people tend to not have this overreaction, they tend to form antibodies fairly rapidly and clear the viral. If you clear the virus very quickly, you’ll actually have very little risk of going into hospital or the ICU. As an aside, if you don’t have a very strong case of COVID-19, looks like you don’t mount a very strong immune response, but that’s another topic for a future discussion. What’s more important is to focus on: What is it about the aging immune system that’s defective that leads to their inability to clear the virus? And then the second part that’s important for the agent is: What happens once they start to clear the virus and why is that so detrimental?
And what we are seeing is that the virus particles, particularly the viral RNA, lasts a long time, sometimes for weeks in the body. And those remnants actually are what we think are stimulating this hyper-immune reaction cytokine storm, which is driven largely by a particular protein complex called the inflammasome, which is already hyperactive, chronically in the agent. And we’ll talk about that later on, but just to give a shout-out to my co-authors, their drawings were beautiful. So we’ll get back to the disease course in a moment. One of the things I want to bring up is one of the great things in this article that Amber and Maeve did was that they drew a table of respiratory viral infections and what are the risk factors? And so I have the table in front of me so I’ll just read off some of them, which you can see in the paper.
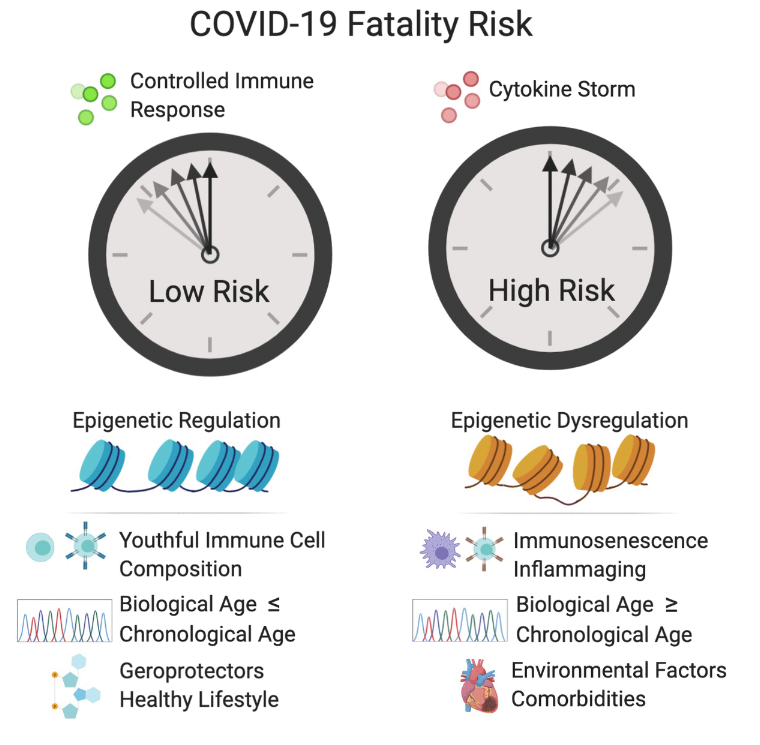
Mers in the original SARS, they actually had high risk. One of the risks was one in Type 2 diabetes, obesity, cardiovascular diseases, hypertension, old age, this is for Mers. For SARS one, it was again diabetes, renal disease, neurological diseases, metabolic, and interestingly dermatological diseases, which is probably an immune thing. But why is that important? What that tells us is that these particular type of corona viruses attack the agent, and in particular, the agent with underlying co-morbidities, these underlying diseases. But what I would like to us to consider and what I’d like to argue is that it’s not just about having obesity, having diabetes, having heart disease that is the problem. Those are symptoms of a more insidious problem, which is that those people are most likely older than their chronological age, or they’re actually very old biologically because they’ve lived a long time, but we know that biological age will be accelerated by being obese, by not exercising and just living the lifestyle that we know from epidemiology is not the perfect one.
At least half of America is overweight or obese. If you include certain cutoffs, some people estimate that it’s over 75% and this drives the aging process. And one of the side effects of course is obesity but obesity may not be the main driver actually, that’s a symptom of the problem that I want to talk to you about. So there are lots of things that go wrong in the aged body. And by age, I’m not just talking about birthday candles, I’m talking about actual biological age. Now biological age can be measured in a variety of ways. Let’s just talk about that for a minute. We can measure the DNA methylation status of ourselves, the so-called Horvath DNA methylation clock, we can measure that pretty easily in a blood test or a swab from the cheek these days get a very accurate estimation of how old someone is biologically.
But there are other things that change in a predictable way. And unlike 10 years ago where we thought we’d never have biomarkers, now we have quite a few. You can look at changes in immune cell diversity, such as T-cells, you can build a very good immune clock. You can look at the levels of NAD in the body, which decline with time. One of the things that we, Gordan Lauc and I, professor Gordan Lauc and I, wrote about is a paper actually also in the journal, Aging, is that the immune system changes in part because sugars change that are attached to proteins. This is the process of glycation and Gordan’s lab has done an amazing job, they’ve found that there’s a glycan clock and what he calls it is the glycogen age of a person.
And why is that important? Because as we get older, the type of sugars that are attached to proteins in the body, whether it’s antibodies or actually the coronavirus spike protein, and even the H2 so-called receptor on the surface of endothelial cells, these are all changed as we get older in terms of their glycation. And if you look at figure 3 in the paper, you can see a beautiful rendition of these changes. And we also have epigenetic changes that control how cells behave. And we know that during aging, epigenetic changes occur, and we think that cells lose their identity. And that’s true for immune cells, it’s true for the lining of the blood vessels, the endothelial cells, and that may be why the virus has a greater chance of attacking an older person’s body as well.
And then finally, there’s the process of immunosenescence. Now that there’s two types of immunosenescence and I don’t want to get people confused here. Immunosenescence typically refers to just the aging of the overall immune system. That means that there’s less variety of T-cells. There’s less ability to mount an immune response and clear viruses, but there’s also cellular immunosenescence or what you call immuno. But there’s also cellular senescence which is a different story, which is about cells checking out of the cell cycle and becoming more like zombie cells. And you can stay in those for galactosidase or p16, and this is another type of cellular senescence.
There’s some overlap between the immunosenescence and cellular senescence, but it’s important to realize they’re not the same thing. And so that’s the lead-up to the whole paper, which goes into detail about these various causes susceptibility to viruses in general, but also to COVID-19. Now, one of the areas that we work on of course are the sirtuins. These are enzymes that our bodies make. There are seven of them in most of our cells, and they’re very important for fighting against diseases, both chronic diabetes, heart disease, Alzheimer’s, we believe based on a lot of mouse and human genetic studies. But also we’re finding are important for viral defenses. And we put forward a hypothesis in this paper that the sirtuin defenses are lost during COVID-19 infections. And one of the reasons for that is the following.
So sirtuins need NAD and unfortunately, as we get older, we think that a lot of our cells lose the ability to make an NAD effectively and they also destroy it for reasons that we don’t fully understand yet. But what we’ve also discovered in my lab and in others, Charlie Brenner put out a nice paper about this a few weeks ago, is that a virus, coronavirus and other types of viruses, deplete NAD in cells. And we think this is part of their defense, the viral attack and the inability of cells to survive the attack. Now they do this through activation of the PARPs. PARPs are poly ADP road to cell trans… polimeracion. So they do this by activating the PARPs, such as PARP1, PARP12, PARP14. And PARPs are enzymes that polymerize NAD and depleted from the cell. And we think that by either blocking the PARP activity or replacing, replenishing the NAD levels in infected cells and in the body of patients, we can give them a better chance of survival.
Now, why would we worry about NAD and sirtuins? Well sirtuins, particularly sirtuin 6, sirtuin 1, sirtuin 2, they control inflammation and they dampen it when it’s overactive. I mentioned the inflammasome. Well, one of the key components of the inflammasome is called NLRP3, and the acetylation chemical to that protein is what causes it to be active. Actually, if we deescalate of enzymes like CERT1, CERT2 deacetylate NLRP3, it brings that activity down. And so what we’re thinking is that when cells are infected, the NAD levels go down. So sirtuins are unable to dampen the inflammatory response and you get this cytokine storm. So in other words, if we were to raise NAD levels in patients, we may be able to prevent their bodies from going into this state of shock and aseptic like response.
Now I will admit, at first I didn’t think this was something that I should rush into. Of course, I would look like somebody with a hammer looking for a nail because you’d think that everything that I do looks like an NAD problem, but studies like the Brown paper that came out as well as studies over the last five years in my lab that have looked at NAD changes during macrophage activation and the PARP response have really pushed me into the belief that, as I write in this article with my coauthors, that NAD is part of this story. Now it’s not the whole story. In fact, the NAD story in this paper is only a small part of it, about 5%, but I want to talk about it because a lot of people are asking me, “David, what about NAD?” And interestingly, I’ve been working with a team in Boston on making an NAD precursor a drug.
And so for the last two years, with the help of a great team at Brigham and Women’s Hospital, they’ve been testing the safety and efficacy of an NAD precursor called MIB626, which is a proprietary version of NAD booster. So far, the molecule is extremely safe in the people that have been tested. It’s able to greatly raise NAD levels. Now there’s some debate out there in the Twitter-verse that the molecules that we work on in my lab and in these clinical trials don’t raise NAD and are not effective. Well, I can tell you that you probably shouldn’t get your scientific information from Twitter because it’s completely wrong. And now what’s interesting and exciting is that in the next few weeks, very extensive, double blind placebo controlled study is about to begin with this molecule. And we’ll see, pretty quickly I think, whether patients are helped by raising an NAD. Particularly the more severe ones.
Now, there are anecdotal case studies already. Some of them are online that you can look up if you’re interested, of patients recovering quite rapidly, supposedly, with treatment with NAD boosters like NMN, which is one of the ones that we work on. But those individual case studies don’t prove anything as we now know from having studied other molecules in other people’s study molecules in the world for COVID-19. So that’s why we’ve decided to do this very rigorous placebo controlled study and not just go for compassionate use. And we’ll see over the next few weeks, perhaps few months, realistically, whether this molecule that we’re working on is going to dampen the inflammatory response in patients that really need it. Drugs are very hard to make, most of them don’t work, so I’m not promising anything, I’m not expecting too much, but I think that we need to give this a shot.
And the other reason for believing in this work is that aging, as I started out in this review, in this talk mentioning, we think aging is the major driver of COVID-19 susceptibility. Aging of all of the different parts of the body in particular, the immune and circulatory systems. Now, if we can delay aging or reverse it, perhaps in some way with NAD boosting or with other drugs that are out there such as Metformin, which [inaudible] is arguing could be used to bring down blood sugar to improve the body’s survival. These kinds of longevity molecules could be used to bring not just the virus down, but boost the survival and the resilience and the defenses of the host up in the same way that you don’t just have weapons of war, you have the defenses as well.
And so on the defensive side, I think bringing up the defenses of the age is just as valid, if not more important than attacking the virus itself. So why would I say, “It’s just as important or more important?” Well consider that this is not the only virus that’s going to attack humanity going forward and vaccines while they’re great and we hold out full on. It probably won’t work against the next outbreak, whether it’s bird flu, regular flu, or another coronavirus, or even a mutated version of this one that’s out in the population. So we need to work also on the body’s ability to fight infections, in general.
So with that, I think I should let you all go. I’ve talked long enough about this paper. I hope you enjoy it. We really enjoyed writing it. It was challenging I’ll admit because it was written in real time as data was coming in and do a lot of things to update. And I’m grateful to Aging, the journal, for making papers available and published within rapid time. And I can tell you that the review process, the peer review process, was extensive. We’ve got pages and pages of comments from reviewers that really helped, particularly in this case. So, enjoy the paper and I’ll keep you updated through my other social media, but also through papers that we hope to publish in the next few months.
Thanks, take care.
Click here to read the full study published by Aging.
WATCH: MORE AGING VIDEOS ON LABTUBE
—
Aging is an open-access journal that publishes research papers monthly in all fields of aging research and other topics. These papers are available to read at no cost to readers on Aging-us.com. Open-access journals offer information that has the potential to benefit our societies from the inside out and may be shared with friends, neighbors, colleagues, and other researchers, far and wide.
For media inquiries, please contact [email protected].
